Red Spots on Roof of Mouth: Causes, Symptoms, and Treatment

Red spots on the roof of your mouth can be a bit worrying, but they are quite common. These spots can show up as tiny dots or larger patches and might hurt or feel fine. It’s important to know what might be causing them, whether it’s an infection, irritation, or something else. In this blog, we’ll take a look at what red spots could mean, what causes them, and how to treat them.
What Are Red Spots on the Roof of the Mouth?
Red spots on the roof of the mouth can appear as tiny red dots, scars, or patches. They may be painless, but in some cases, they’re accompanied by soreness, swelling, or discomfort. While red spots might be harmless and go away on their own, they can also indicate infections, allergies, or even a response to irritation.
Red Spots on Roof of Mouth Pictures
Here are some pictures of red spots on roof of mouth:


Symptoms
In addition to red spots, other symptoms can give clues about the cause:
- Pain or Soreness: Some red spots are painful, especially if caused by infections or irritation.
- Swelling or Blisters: Red spots may be accompanied by swelling or small blisters, indicating possible allergies or infections.
- Persistent Spots: Red spots lasting over two weeks might indicate a more serious underlying issue.
What Causes Red Spots on Roof of Mouth?
The most common causes include infections, environmental factors, and some underlying health conditions.
Infectious Causes
Viral Infections: Cold sores (herpes simplex virus) and canker sores often cause red spots or sores in the mouth.
Bacterial Infections: Bacterial infections like strep throat may cause red spots and require antibiotics.
Fungal Infections: Oral thrush, a fungal infection, can lead to red and white patches in the mouth.
Autoimmune and Systemic Causes
Oral Lichen Planus: An autoimmune condition that leads to red or white lacy patches in the mouth.
Blood Disorders: Conditions like leukemia can cause red spots due to reduced blood platelets, leading to bleeding in the mouth.
Kawasaki Disease: A rare but serious condition, especially in children, that causes red spots along with other symptoms like fever and swollen lymph nodes.
Mouth ulcers (canker sores): Often associated with the immune response and may be triggered by factors like stress, certain foods, or underlying health conditions.
Environmental Causes
Allergic Reactions: Foods, mouthwashes, or toothpaste ingredients can cause allergic reactions, leading to red spots.
Injury or Irritation: Hot foods, hard foods, or using a hard-bristled toothbrush can cause small injuries, resulting in red spots.
Smoking or Tobacco Use: Tobacco can irritate the mouth’s soft tissues and is a significant risk factor for erythroplakia, which may present as red spots or patches in the oral cavity.
What Does an Infection on the Roof of the Mouth Look Like?
Infections in the mouth may appear as red or white spots, small blisters, or patches. They are often accompanied by symptoms like swelling, pain, and sometimes a burning sensation. Viral infections like cold sores or bacterial infections like strep throat are often marked by clear red spots with or without pain.
How Do I Get Rid of Red Spots on the Roof of My Mouth?
Treatment depends on the cause.
- For Infections: Viral infections often clear on their own, while bacterial infections like strep throat need antibiotics. Oral thrush (fungal infection) requires antifungal medication.
- For Allergies: Avoiding known triggers and using antihistamines can help with allergic reactions.
- For Minor Injuries: Rinsing with salt water can soothe the area, and avoiding hot or spicy foods allows it to heal faster.
Home Remedies to Soothe Red Spots
Here are a few easy, at-home remedies that might help relieve discomfort:
- Saltwater Rinse: Mix a teaspoon of salt with warm water, swish for 30 seconds, and spit out. This can soothe inflammation and help with healing.
- Cold Compress: Applying a cold pack to the outside of your mouth may reduce pain and swelling.
- Honey: Known for its natural antibacterial properties, a little honey applied to the area may offer soothing relief.
- Avoid Hot or Spicy Foods: These can irritate red spots and make them more painful.
Diagnosis
If red spots persist, a healthcare provider may:
- Perform a physical examination and check for symptoms like swelling, soreness, or any unusual changes.
- Order a swab test or culture if an infection is suspected, which can identify bacteria, viruses, or fungi.
- Suggest blood tests if a systemic condition like a blood disorder is suspected.
Treatment
Treatment for red spots varies based on the diagnosis.
- Medications: Antibiotics for bacterial infections, antifungals for thrush, or antivirals for cold sores.
- Lifestyle Adjustments: Avoiding spicy foods, using a soft-bristled toothbrush, and drinking plenty of water can prevent further irritation.
- Topical Treatments: Over-the-counter ointments or mouth rinses can reduce pain and inflammation.
How Can Red Spots on Roof of Mouth Be Prevented?
- Good Oral Hygiene: Brushing and flossing regularly can reduce bacteria buildup.
- Stay Hydrated: Drink water throughout the day to keep your mouth moist and prevent irritation.
- Use Mild Dental Products: Choose toothpaste and mouthwash with gentle ingredients if you have sensitive gums or experience frequent irritation.
- Avoid Known Allergens: If you have food allergies, avoid those items and check product labels to prevent reactions.
When to Contact a Healthcare Provider
Seek medical advice if:
- Red spots persist for more than two weeks.
- You experience significant pain, swelling, or difficulty swallowing.
- The spots reoccur frequently or are accompanied by symptoms like fever, weight loss, or fatigue.
Conclusion
In simple terms, red spots on the roof of your mouth can happen for many reasons, and most of the time, they aren’t severe. However, if they last too long or hurt a lot, it’s wise to check with a doctor. Keeping your mouth clean and being careful with what you eat can help avoid these spots. If you’re ever worried about your mouth, don’t hesitate to talk to your dentist for advice!
Dry Socket vs Normal Socket : Causes, Symptoms and Treatments

Tooth extractions are common dental procedures, but the healing process can vary significantly depending on whether a normal or dry socket develops. A normal socket forms as a healing cavity where the tooth is removed, characterized by a blood clot that protects the underlying bone and nerves, aiding in healing. In contrast, a dry socket is a painful complication that occurs when the blood clot is lost or fails to form, exposing the bone and causing intense discomfort. This blog will explore the key differences between normal sockets and dry sockets, including their healing processes, symptoms, causes, treatments, and prevention strategies.
Normal Socket After Tooth Extraction
A normal socket after tooth extraction is the healing cavity left in the gum where the tooth was removed. It is characterized by the formation of a blood clot that protects the underlying bone and nerves. This clot is essential for healing, as it prevents infection and allows new tissue to regenerate. In a normal socket, patients typically experience mild pain and swelling, which gradually decrease as the socket heals over the following weeks to months.
Healing Normal Socket After Tooth Extraction
After a tooth is extracted, the socket heals step by step. First, a blood clot forms in the empty socket, which helps protect the bone and nerves underneath. Over the next few days, the gum tissue starts to close up, and the pain begins to decrease. Within a week or two, the socket continues to heal as new tissue grows. After about a month, the bone starts filling in the space, and the soft tissue usually finishes healing. Complete bone healing may take a few months, but with proper care, the recovery should be smooth and uncomplicated.
Causes of Normal Socket
A normal socket forms after a tooth extraction is done. This healing cavity is essential for recovery and is influenced by several causes:
- Successful Tooth Removal: A careful and smooth extraction minimizes damage to surrounding tissues, promoting better healing.
- Blood Clot Formation: The socket experiences a blood clot right after the extraction. This clot is important because it shields the nerves and bone underneath.
- Good Blood Flow: Healthy blood circulation delivers important nutrients and oxygen to the area, which aids in the healing process.
- Body’s Healing Response: The body’s natural healing mechanisms work to repair the area, preventing infection and encouraging new tissue growth.
Symptoms Of Normal Socket
Symptoms of a normal socket after tooth extraction typically indicate that the healing process is proceeding well. These symptoms include:
- Mild Pain: Some discomfort is normal, but it should be manageable and gradually decrease over a few days.
- Swelling: Mild swelling around the extraction site is common but should start to diminish within a few days.
- Soreness: The area may feel tender, especially when touched, but this should improve as healing progresses.
- Normal Bleeding: Some bleeding may occur immediately after the extraction, but it should stop within a few hours. Any residual blood should be minimal.
- Closure of the Socket: Over time, the socket should gradually close up as new tissue forms over the area
How To Treat Normal Socket?
Here are treatment tips for a normal socket after tooth extraction:
- Saltwater Rinse: Gently rinsing with warm salt water helps keep the area clean and aids healing.
- Avoiding Straws: Using straws can dislodge the blood clots and prevent them for the first few days.
- Cold Compress: Applying a cold compress can help reduce swelling and pain.
- Soft Foods: Eating soft foods prevents irritation of the socket and promotes healing.
- Good Oral Hygiene: Maintain good oral hygiene, but avoid brushing directly on the extraction site for a few days to prevent irritation.
- Stay Hydrated: Drink plenty of fluids to stay hydrated, but avoid hot drinks for the first few days.
What is Dry Socket?
A dry socket, also called alveolar osteitis, is a painful dental condition that can occur after a tooth extraction, especially from the wisdom teeth. Normally, a blood clot forms in the tooth socket to protect the bone and nerves as the area heals. In the case of a dry socket, the clot either dissolves or becomes dislodged, leaving the underlying bone and nerves exposed. This leads to intense pain, delayed healing, and often a bad taste or odour in the mouth.
Symptoms Of Dry Socket After Tooth Extraction
Symptoms of dry socket (alveolar osteitis) after tooth extraction can include:
- Severe Pain: Intense pain that typically starts 2-4 days after the extraction and can radiate to the ear, eye, or side of the face.
- Empty Socket:An absence of a blood clot in the socket, which may appear dry or empty.
- Bad Breath: A foul odour coming from the extraction site.
- Unpleasant Taste: A bad taste in the mouth due to the exposure of the bone.
- Swelling: Possible swelling around the extraction site.
- Delayed Healing: Slower than expected healing of the socket.
Causes of Dry Socket
Dry socket (alveolar osteitis) can occur due to several factors, including:
- Dislodged Blood Clot: If the blood clot that forms in the socket is dislodged or dissolves prematurely, it can lead to a dry socket.
- Inadequate Blood Supply: Conditions that affect blood flow to the extraction site can increase the risk of dry sockets.
- Smoking: Tobacco use can interfere with blood clot formation and healing, increasing the likelihood of dry sockets.
- Infection: Bacterial infections at the extraction site can disrupt the healing process and lead to complications.
- Hormonal Changes: Hormonal fluctuations, particularly in women (e.g., during menstruation or hormone therapy), may affect healing and increase the risk.
- Trauma to the Socket: Activities that disturb the extraction site, such as vigorous rinsing or spitting, can dislodge the blood clot.
- Poor Oral Hygiene: Insufficient oral care can lead to infections and complications during the healing process.
- Complex Extractions: More complicated extractions, such as those involving impacted wisdom teeth, can have a higher risk of dry sockets due to increased trauma to the surrounding tissues.
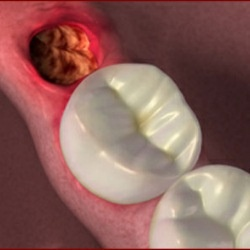
How Does Dry Socket Look Like?
A dry socket, a common complication after tooth extraction, occurs when the blood clot protecting the extraction site is dislodged or dissolves prematurely. This leaves the bone and nerves exposed, leading to intense pain and delayed healing. Visualizing a dry socket after tooth extraction pictures can help identify its appearance and differentiate it from normal post-extraction healing.


How To Treat Dry Socket?
- Flushing Out the Socket: A dentist may gently flush the socket to remove debris and bacteria.
- Dental Intervention: Cleaning the socket and possibly placing medicated dressings to promote healing and alleviate pain.
- Pain Management: Prescription pain relievers may be necessary to control severe discomfort.
- Antibiotics: May be prescribed to manage or prevent infection, especially if there are signs of complications.
- Self-Care: Patients can maintain oral hygiene by rinsing with warm salt water (as directed) to reduce the risk of infection.
Preventing Dry Socket After A Tooth Extraction
Here are some tips for preventing dry socket after a tooth extraction, including the importance of proper oral hygiene:
- Avoid Smoking and Tobacco: Refrain from smoking and using tobacco products for at least 48-72 hours after the extraction, as they can hinder healing and dislodge blood clots.
- Avoid Straws: Don’t use straws for at least a week after the extraction, as the suction can dislodge the blood clot.
- Maintain Proper Oral Hygiene: Gently brush your teeth while avoiding the extraction site to keep your mouth clean and reduce the risk of infection.
- Eat Soft Foods: Stick to soft foods for the first few days post-extraction, avoiding hard, crunchy, or hot foods that can irritate the socket.
- Use Pain Medication as Directed: Take any prescribed pain medication to manage discomfort, which can help you avoid inadvertently disturbing the extraction site.
Dry Socket vs Normal Socket
The main difference between dry socket pain vs normal pain after tooth extraction is that a normal socket features a stable blood clot that protects the underlying bone and facilitates healing, while a dry socket occurs when the blood clot is dislodged or fails to form, exposing the bone and resulting in severe pain and delayed healing. Here are some key differences listed:
| Feature | Normal Socket | Dry Socket |
| Definition | Socket healing with a blood clot | Complication where the blood clot is dislodged or absent |
| Pain | Mild to moderate pain that decreases over time | Severe, sharp pain that begins a few days post-extraction |
| Healing Process | Clot present, socket may appear reddish | Empty, dry socket with exposed bone visible |
| Swelling | Mild swelling around the extraction site | Increased swelling in the area |
| Odor | No significant odor | Foul odor due to bone exposure |
| Taste | Normal taste, no unpleasant sensations | Bad taste in the mouth due to exposed tissue |
Pictures of Dry Socket vs Normal Healing

Conclusion
Understanding the difference between a normal socket and a dry socket is important after tooth extraction. A normal socket heals with little discomfort, while a dry socket can cause severe pain and complications. Knowing the signs of each, following care instructions, and taking precautions can help ensure a smooth recovery. If you have severe pain or signs of a dry socket, see your dentist right away for treatment. With proper care, you can heal well and reduce the chance of complications.
Does Smoking cause receding gums?

Smoking has long been linked to several health issues, including damage to the gums. Recent studies have suggested that Smoking could contribute to receding gums. It is a condition where the gum tissue around the teeth begins to pull away, leading to further dental problems. This blog post will explore the connection between smoking and receding gums and discuss the implications for oral health.
Read More…How to deal with loose fillings?

The insertion of tooth fillings is a widely performed treatment to repair decayed teeth. The procedure involves evacuating the decayed or damaged portion of a tooth and the space is filled with dental filling materials. The fillings are a single or combination of different materials that can restore the sturdiness of a tooth. Likewise, it can prevent the progression of cavities.
Even though the cavity fillings are highly durable, they become loose over time due to constant wear and tear. Such loose fillings should get immediate fix because the consequences of loose or dislodged fillings are more detrimental.
How can you identify loose fillings in a tooth?
Read More…Why do you have black gums around your teeth?
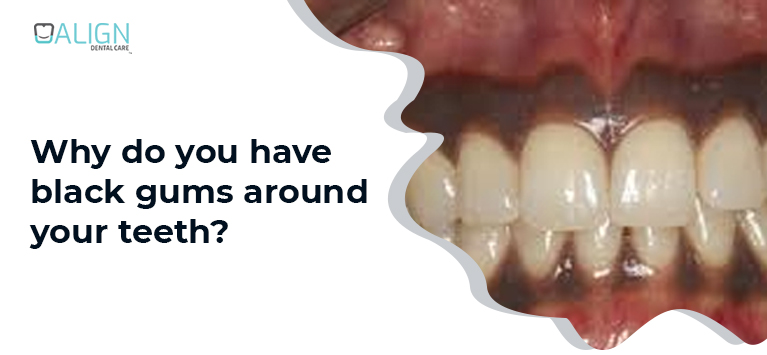
Pale pink is the natural color of the gum tissues surrounding our teeth. Even though the gum color varies for each person, dark colored gums ruin your smile aesthetics because an optimal interrelation between teeth, gums, and other oral tissues is essential for a beautiful smile.
Mostly, hormonal changes make your gums turn a different color. On the other hand, gum discoloration is a sign of underlying bodily disorders.
Read More…Why do I have pain in teeth and gums after flossing?

Flossing is an essential part of everyone’s oral care routine as the flossing wire is capable of cleaning tiny spaces between the teeth where the brush bristles cannot reach. Do you notice any pain in or around your teeth after flossing? Don’t worry. It is pretty usual, especially for people who just begin flossing whereas such flossing ache implies some underlying dental problems.
If you want the answer to the question “Why do I have toothache after flossing?”, Keep reading this post. We have explained the possible causes of such flossing ache.
Read More…What Everybody Ought to Know About Tongue-Tie?
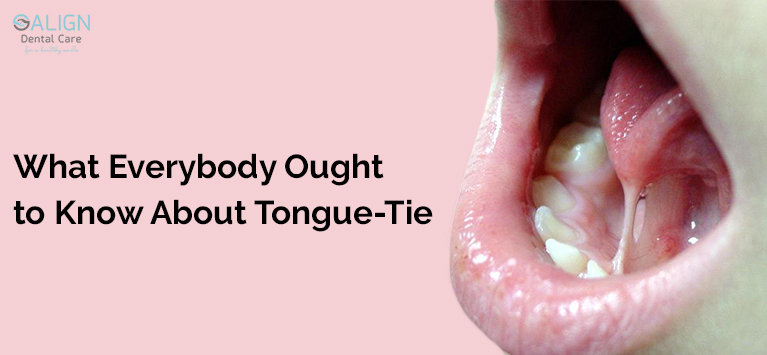
The underside of our tongue is connected to the floor of the mouth with a fold of tissue called lingual frenulum. In general, the tissue is thick and becomes thin, stretchy after delivery. In certain cases, the tissue remains thick and restricts tongue movements. This condition is called Ankyloglossia.
Such tongue-tie affects the baby’s ability to latch efficiently during breastfeeding. Similarly, it intervenes in the infant’s speech articulation, making them hard to pronounce some letters.
Read More…How does common cold affect your oral health?

Common cold seems a normal problem and exhibits symptoms like runny nose, cough, congestion and sore throat. In general, every adult gets cold 3 to 4 times a year whereas kids have 6 to 10 times. In certain cases, flu and common cold persists for more than a week and hurt pain and teeth. Keep in mind that such oral complications when you have cough are warning signs of harmful diseases.
In this article, we have explained the impact of cold diseases on our dental health and simple tips to overcome the difficulties.
Read More…Top summer foods for healthy teeth

Summer is nearing fast, and it will start in a new period of berries, vegetables, and different foods. Have you thought the summer foods are great for your oral health while you are on the beach, on the road, or at a picnic?
Below are a few summer foods that are healthy for your teeth.
FRUITS
Lots of new summer fruits will soon consume the grocery store’s section of food. Here are a few good ones that will improve your oral health. Please remember that the mentioned fruits are acidic, and may break down your teeth’s enamel. Wash it with a glass of water while eating on such fruits or consume them with minimal-acid foods, such as a handful of almonds.
Apples
Although most apples are picked in fall, some varieties are grown in summer.
Yellow Transparent Apples
Earligold Apples
Jersey Mac Apples
Gala Apples
Lodi Apples
Consuming an apple increases saliva production, which acts to wash away bacteria and food particles. Apples have a high content of water, which helps to dissolve the sugar they incorporate. It’s harder texture enhances your gums as well.
Strawberries
Strawberries, high in vitamin C, help minimize inflammation and produce collagen, a protein that aids combat periodontal disease. Strawberries, high in vitamin C, help minimize inflammation and produce collagen, a protein that aids combat periodontal disease. This fruit contains even calcium, which encourages healthy bones and teeth.
Peaches
This traditional summer fruit holds fluoride, which is an essential dental-health mineral. Fluoride enables the remineralization and reconstruction of enamel while improving your existing enamel. In the end, this helps avoid the development of cavities. Peaches too are filled with vitamin C, which helps to reduce inflammation. They already constitute calcium, which fortifies teeth and bones. Before consuming a peach, please ensure you eliminate the pit, since chewing on a pit will harm your teeth.
LEAFY GREENS
Butter lettuce is a famous leafy green in the summertime. This kind of lettuce comprises vitamin A which produces enamel of the teeth. It too has tiny quantities of calcium, which reinforces your teeth and bones.
CHEESE
There are also seasonal cheeses, like vegetables and fruits. Goats and sheep give milk only in summer and spring, presenting these cheeses the freshest options in season:
Feta Cheese
Goat Cheese
Ricotta
Mozzarella
In cheese, the calcium and protein help to reinforce the teeth and bones. Chewing cheese’s action is often believed to promote the production of saliva, cleaning the bacteria and food particles in your mouth.
FISH & MEATS
Igniting up the grill is a perfect summer activity, but for your oral health, it’s also a smart step. Meats are protein-rich and comprise phosphorus. This assist fortifies the jaw and teeth. To enhance the health advantages of the summer cookout, select lean meats, such as turkey and chicken. Fatty fish comprise Omega-3 fatty acids which were observed to reduce the hazard of developing gum disease in studies.
Eggs/Beans
Another origin of phosphorus is eggs, so go forward and add heavy-boiled or stuffed eggs to your upcoming cookout as a side dish. Make stuffed eggs instead of mayonnaise with Greek yogurt and low-fat cream cheese. Beans are yet another high-fiber food, such as raw vegetables, which takes a lot of chewing, which also enhances saliva.
Many different types of snacks and foods encourage dental health. Eliminate eating sticky foods that are challenging to brush your teeth and don’t binge on sugary snacks all day long.
Denture care tips and guidelines

Whether full or Partial dentures, keeping them safe and free from stains and bacteria requires routine, appropriate care. Proper care will keep both the mouth and dentures in perfect condition. These useful tips describe the way your dentures are washed, handled, and stored correctly.
Cleaning Dentures
After the meals remove and rinse the dentures. If, after every meal, you are often not able to wash your dentures, at least make sure to rinse and brush them with a denture cleaner, soft dish soap, or liquid soap once a day to eliminate plaque, food, and other contaminants.
Clean any remaining adhesive off your gums if you are using a denture adhesive. Do not use a denture cleanser for this purpose. Brush the natural teeth and clean the tongue, mouth roof, and cheeks. Soak the dentures overnight in the solution. Your dentist or solution company will have their own suggestions so please follow instructions.
Several things to clean dentures you should never use include:
Whitening toothpaste
Toothpaste will be completely abrasive with teeth whitening properties. Don’t use it for denture cleaning.
Abrasive cleaning items
Heavy-bristled toothbrushes and rough cleaners and toothpaste are much too abrasive and may cause severe harm to dentures.
Hot water
In relation to sterilizing the dentures, they may be damaged by hot water.
Bleach Products
Bleach damages dentures and alters color. The metal components in the dentures with metal links can also be tarnished by solutions that contain.
How to handle dentures?
Wash them completely before putting the dentures back in, particularly if you are using a cleaning solution. When swallowed, the toxic chemicals in the solution may cause vomiting, discomfort, or burning. Dentures are quite fragile and can easily break when dropped. Often keep them above a soft towel while handling the dentures, or load your sink with water.
Storing dentures
If dried out or are put in hot water, the dentures may become warped. Your dentures must either be kept in water with room temperature or in a denture solution suggested by your dentist while you are not using them.
Never cover the dentures in a towel of paper. They may easily be confused with waste, then thrown away. Keep your dentures much out of reach of children and pets and keep them safe. Children enjoy playing with dentures and dogs enjoy chewing them up.
Schedule routine dentist appointments to have your teeth and dentures tested and cleaned. If you feel dentures are loose, immediately consult your dentist.